I write this post as someone who has successfully overcome prolapse and who now treats other women with it, and I can tell you there is so much hope.
Prolapse (POP) is often a scary diagnosis, and I vividly remember being scared myself when I stood in the office of my OB and begged him to tell me that nothing would fall out. (He actually responded with “well, it does sometimes,” which was terrifying and entirely unhelpful, and in hindsight, I realize he needed to read “Words that Harm, Words that Heal” for better communication with patients). He sent me to PT, although my first attempt at rehab was not successful and it took finding the right PT to get the comprehensive evaluation and treatment that I needed to truly recover. That also started my own journey to becoming a women’s health provider, which you can read more about here.
Back to prolapse, which literally means “to fall out of place.” Prolapse is caused by a stretching of the ligaments and muscles that support the pelvic organs, causing those organs to dropdown.
What causes POP?
Anything that puts pressure down on the pelvic floor including:
- Pregnancy and childbirth
- Heavy lifting
- Constipation and straining to stool
- Breath-holding during physical effort
- Lung disease and chronic cough
- Pelvic surgery
- Obesity
- Postmenopause
Symptoms of pelvic organ prolapse
- Aching or heaviness in the pelvis
- Bulging or swelling in the vagina
- Pain with intercourse
- Straining to urinate, or incomplete bladder emptying
- Difficulty passing stool
- Bladder or bowel incontinence
- Back pain
- Abdominal pain
- Hip pain
As someone who has suffered with significant prolapse, and recovered, I can tell you that it is not as scary as it sounds! There are several types and grades of severity for each type.
- Urethrocele: the urethra prolapses down
- Vaginal prolapse: the walls of the vagina become overstretched and bulge down/in towards the vaginal opening.
- Uterine prolapse: the uterus drops down towards the vaginal opening.
- Bladder prolapse (also called cystocele): the bladder drops down and pushes against the front of the vaginal wall, creating a bulge towards the vaginal opening.
- Bowel prolapse (also called rectocele): the bowel drops forward and pushes against the back of the vaginal wall, creating a bulge towards the vaginal opening.
Any one type can occur along with another. There are different levels of severity from grade 1 (just a little bit of drop-down) to grade 4 (things have actually fallen out). There actually isn’t as much of a correlation as you would think between severity and symptoms as far as pain, achiness, heaviness, and difficulty functioning, however, there is some association. That is one reason that PT is so helpful; I have seen women with grade 3 and minimal symptoms, and women with grade 1 or 2 and significant symptoms. We know we can treat the women with grade 1 or 2 POP, and I see a lot of success with grade 3 as well. I have also seen women with grade 4 POP who choose not to have surgery and manage well enough with PT alone, although most women with grade 4 do choose surgery.
Sidebar
| Even if you have had surgery, or plan to, rehabilitation both before (prehab) and after surgery will lead to the best outcomes. This is another sorely neglected area of care for women. I’ve seen women several years after their surgery when symptoms popped up again, and they have been shocked at their improvement with PT and wondered why they hadn’t known to try it before. |
The cause of each type is most commonly weakness or loss of integrity in the supporting structures of the pelvic floor: muscles, ligaments, and fascia. These structures work together to form what we refer to as a hammock of support for the pelvic organs. Loss of coordination between the pelvic floor muscles and the other core muscles is also a huge contributing factor and the one that is most commonly ignored by traditional medical interventions.
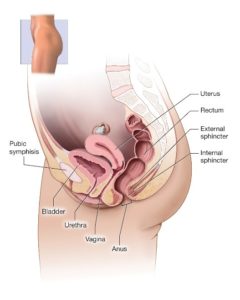
Female Pelvic Organs, source: womenshealth.gov
There is much hope for women with prolapse
It is very common postpartum (possibly existing in 100% of women in the early postpartum weeks according to some experts), and we like to see it resolve by 3 months postpartum. It is one reason that a postpartum physical therapy visit is so important, typically at 6-8 weeks. Prolapse needs to be identified early and addressed appropriately. Some women are more likely to have prolapse due to pregnancy and labor and delivery factors, as well as genetics (mostly due to genetic makeup of connective tissue and muscle tone). Through physical therapy, most women can improve their prolapse, sometimes completely or sometimes enough so that they don’t have symptoms or limitations in function. In more significant cases, surgery may be indicated. I am happy to say that that is rare in my practice. It is very important to know that the failure rate of prolapse surgery is rather high, some experts report that 1/3 surgeries fail, and some experts report that the mesh has a lifetime of 5 years (meaning more surgery could be needed). Of course technology is always improving, and I can refer you to excellent physicians if needed.
Sidebar:
|
Currently, almost half of women have a lifetime incidence of prolapse. How can we improve this stat? Through postpartum physical therapy for one. In other countries, postpartum physical therapy is standard care. Let’s make that true here in the US for all women! The pelvic floor goes through an incredible feat and deserves all the healing we can give it. Awareness is also key, especially in the fitness industry where technique or form may contribute in susceptible individuals.
|
What can’t I do?
I am very disappointed when I hear that women were told that they can’t do something because of their POP…because usually they can! What that typically means to me is that they need a better evaluation and treatment. It may be true that initially, it is necessary to avoid certain exercises or activities. However, with the right training, women with POP can go on to lift heavy things and exercise hard. They might have to put in some hard work to retrain their body, but it can often be done.
How can PT help with POP?
Treatment of prolapse involves an individualized, thorough approach. It typically includes assessment and treatment of pelvic floor muscle flexibility, strength, and activation. Sometimes the pelvic floor muscles are underactive, or not firing quickly enough to support the pelvic organs during movement. Sometimes the pelvic floor muscles are overactive, meaning they are “on” all the time, which means they can fatigue too quickly to provide adequate pelvic organ support during movements with higher demands. Either way, the pelvic floor muscles can be retrained to be stronger and to fire at the right time in coordination with the other core muscles. Treatment also involves evaluation of the spine, pelvis, and hips. A huge factor in prolapse is control of intraabdominal pressure, which may be excessive and cause too pressure down on the pelvic organs if we have abnormal posture or faulty movement mechanics. If the abdominal muscles tend to “grip” or be overactive, that can put a tremendous amount of pressure down. So can tucking your bum, or “glute gripping.” Even thoracic (upper back) stiffness can play a role in control of pressures and worsen prolapse. How we use our diaphragm and breathing mechanics also have a role to play in management of prolapse. Any abdominal tightness or scar tissue from a surgery or endometriosis can also play a key role. As you can see, a comprehensive approach is required. The research is very supportive of PT for mild to moderate prolapse. Working one on one with a physical therapist is more effective than using an online program. It does take time, and dedication to the exercises. Your exercise program will start out with fairly simple and easy, low weight exercises, and progress as your body is able to handle more load. Initially, we might even use inverted positions that allow gravity to assist in relieving symptoms and give the muscles a better chance to fire. Most of the time patients are unaware of postures and movements that are provoking symptoms, but that postural awareness can be retrained. Many people can get back to handling heavy loads, or even perform higher than ever before due to optimizing their core control (this was my personal experience). For some, however, there can be limitations based on several factors including the degree of POP and the body’s individual response.
Can’t I just do Kegels?
3 out of 4 people actually do Kegels (pelvic floor muscle contractions) incorrectly without personalized instruction. Even when taught verbally, most people struggle to get the pelvic floor muscles to effectively squeeze and lift in coordination with the other core muscles. And, Kegels might not be the right exercise for your POP if you have overactive pelvic floor muscles, which is surprisingly common in patients with POP. In that event, just doing more Kegels could cause your symptoms to worsen. Learning how to fully relax and contract the pelvic floor is very important. In some cases, the pelvic floor muscles have appropriate strength and activation, but the forces around them are the cause of the POP due to overuse of the abdominals, or postural forces contributing to excessive intraabdominal pressure. Your patterns of movement and postures have to be changed to better manage pressures. Whole-body strength is then important to build, using the new patterns of movement that you learn. That sounds challenging, and it can be, but I am completely honest with you when I say if I can do it, anyone can.
Don’t wait, see a specialist
Regardless of whether you have prolapse during pregnancy, postpartum, or not until menopause, or even if you haven’t had children but have another cause such as weight lifting or chronic asthma, there is hope for you too. You shouldn’t be limited in your daily activities or fitness goals and a good physical therapy plan can get you back to the life you desire.
|
Tips for management of POP: · Weight management · Avoid straining (when lifting, urinating, or stooling) · Constipation management: hydration, moderate fiber, and squatty potty · Stay active but avoid activities that reproduce symptoms pending PT evaluation · Avoid breath-holding with effort (Valsalva) |





