What if your low back pain isn’t just a low back problem?
80% of people will have low back pain at some point in their lives!
How many of you have had back pain at some point, or have a friend or family member that struggles with it on and off? Sometimes it is just a little annoying, and sometimes it is a major hindrance. Not only can it put a damper on our ability to function, but it is associated with skyrocketing healthcare costs.
Good News!
Physical Therapy has been shown to help resolve, manage, and prevent low back pain! In many studies, PT helps as well or better than drugs and surgery.
| There are a few large medical centers in the US that have studied using PT as the frontline provider for patients with low back pain, which then led to decreased rates of surgery and medicine use, decreased use of imaging, and decreased surgical rates, along with improved pain and function outcomes at one year! (If you are interested, Virginia Mason Medical Center is one such example). |
Why does low back pain recur?
Sometimes people try physical therapy and don’t experience the relief they need. Likely, they need to try another physical therapist. Or, sometimes people let their busy-ness get in the way of finishing therapy: don’t drop out as soon as you experience relief. Hang in there and finish rehab until you are 100% better! But often, if PT hasn’t worked for someone, a more thorough evaluation of contributing structures is indicated. That’s what this post is really about…often back pain recurs because it is often not just a low back problem. In fact, one study showed that 95% of women who presented to PT with lumbopelvic pain had pelvic floor dysfunction! This included pelvic tenderness (71%), weakness (66%), and pelvic organ prolapse (41%).1 There may be other contributing structures as well such as the upper back, hips, knees, and feet. However, we are going to focus on the pelvic floor for this post because it is a huge missing link.
Other studies have looked at the relationship of chronic low back pain to pelvic floor dysfunction, particularly stress urinary incontinence, and have also shown a strong link. Because this research is relatively new, not every orthopedic physical therapist is going to screen for pelvic floor issues. Fortunately, the number of general PTs and primary care providers that do ask questions about those issues is rising. Even then, patients may not disclose what seems like an “embarrassing” or “personal problem” to a “regular” therapist. We hear that often from our colleagues. But many PTs do screen for it, and many of our patients come from physical therapists in the area that are referring them for evaluation of their pelvic floor. Incidentally, the same is true for hip problems…quite often the pelvic floor is involved.
|
How do you know if you need to go to the physician or get imaging? MRIs have not been shown in research studies to correlate well with patient symptoms or to assist in the selection of treatment interventions for back pain. More commonly they show age-related changes, or “wrinkles on the inside.” With the increase in advanced imaging such as MRIs, we have also seen a correlated increase in surgery and opioids, but unfortunately not better outcomes for most people. You should know that only a very small number of people have a major issue causing their pain that may need imaging, and PTs are highly trained in screening for red flags that may indicate a serious condition. You do not have to see a physician before seeing a physical therapist. |
| Of women with low back pain, more than 95% had pelvic floor dysfunction as well! (Dufour, et al 2018). This included pelvic tenderness (71%), weakness (66%) and pelvic organ prolapse (41%). |
Why is pelvic floor dysfunction possibly related to your back pain?
The pelvic floor muscles are the “floor” of the all-important core. They are particularly important for not only control of bladder and bowel function but also for support of pelvic organs, sexual function, and core stability. These muscles work in concert with the other core muscles, including the diaphragm, the deep abs, and the deep back muscles to support the spine and give us controlled movement. Did you know that the first muscle group to fire when you raise your arm up is actually the pelvic floor? The fancy name for this is anticipatory core control: the brain anticipates movement and calls on the deep core muscles for stability first.
When injury or pain occurs, the teamwork of the core muscles is often disrupted. Pregnancy and childbirth decrease the coordination and function of our core, as do abdominal or back surgery. Back or hip injury may also disrupt the function in any of the core muscles. So may bladder, colon, uterus, or ovarian pain. The pelvic floor muscles may be weak, tight, underactive, or overactive. They may not be responding as quickly as they should or they may be “on” all the time, (overactive) contributing to painful trigger points, due to the body’s attempt to create stability or due to a person’s tendency to hold stress in the pelvis (just as one might carry stress in the neck and upper shoulders). In someone with pelvic floor symptoms, whether that is the cause or the result of low back pain is very individual. In such cases, treating both areas will result in the best outcomes and the happiest patients. If pelvic floor impairments are not addressed, a cycle of dysfunction can develop, leading to persistent or recurrent low back pain.
What are pelvic floor symptoms that might relate to your back pain?
The most common related symptoms may be obvious or subtle, and may include:
- Stress urinary incontinence
- Bladder urgency or frequency
- Painful intercourse
- Constipation
- Prolapse (a feeling of heaviness in pelvis or a falling out feeling)
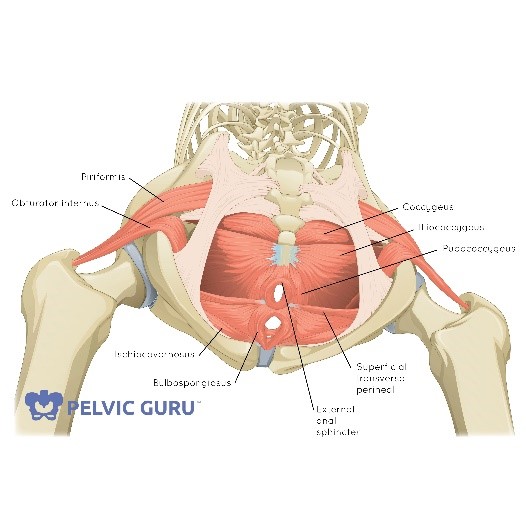 First image: The 3 layers of pelvic floor muscles, and attachments into the base of the spine. Image used by permission of Pelvic Guru, LLC.
First image: The 3 layers of pelvic floor muscles, and attachments into the base of the spine. Image used by permission of Pelvic Guru, LLC.
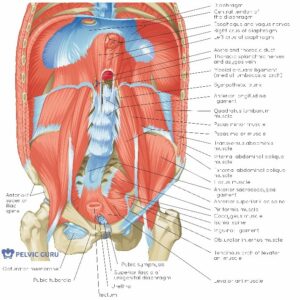 Second image: The pelvic floor, the diaphragm, the hip, and some of the spinal muscles attaching into the pelvis and the spine. Image used by permission of Pelvic Guru, LLC.
Second image: The pelvic floor, the diaphragm, the hip, and some of the spinal muscles attaching into the pelvis and the spine. Image used by permission of Pelvic Guru, LLC.
Can physical therapy help with this? The good news is…
Absolutely. We see patients all the time with any combination of pelvic floor dysfunction, back pain, SI pain, tailbone pain, and/or hip pain. Using a holistic approach, we evaluate the pelvic floor and surrounding regions and determine how different areas are affecting each other. One recent patient who had 10 years of back pain experienced complete relief when her pelvic floor symptoms were evaluated and treated. We see cases like this all the time.
At Integral PT, we use a holistic, individualized, thorough approach to pelvic floor dysfunction that includes assessment and treatment of the back, hips, and other areas that may be related to your symptoms. We also work in collaboration with referring physical therapists and provide the pelvic floor portion of the treatment plan.
Do you have unresolved or recurrent back pain?
Don’t use a “wait and see” approach, contact us today and schedule an evaluation of any low back or pelvic symptoms that you are having! And knowing how many women this affects, share this post and spread the word to help someone else feel better.
- Darfour S, et al. Association between lumbopelvic pain and pelvic floor dysfunction in women: a cross sectional study. Musculoskeletal Science and Practice. 2018;24:47-53.





